Vaginal atrophy during menopause is common—but manageable. Explore 7 empowering, science-backed strategies to treat and manage symptoms naturally and effectively.
📚 Table of Contents
- Understanding Vaginal Atrophy During Menopause
- Common Symptoms of Vaginal Atrophy
- What Causes Vaginal Atrophy During Menopause?
- 7 Empowering Ways to Treat and Manage Vaginal Atrophy
- Medical Treatment Options for Vaginal Atrophy
- When to Talk to a Healthcare Provider
- You Deserve Comfort and Confidence
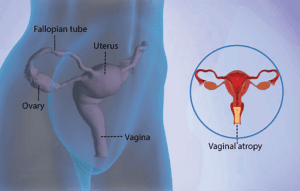
1. Understanding Vaginal Atrophy During Menopause

Alt text: Diagram showing vaginal atrophy during menopause
Vaginal atrophy during menopause, also known as genitourinary syndrome of menopause (GSM), refers to the thinning, dryness, and inflammation of the vaginal walls caused by decreasing estrogen levels.
At MenoThrive Wellness, you deserve access to honest information and supportive tools that empower you to control your body and wellness journey.
2. Common Symptoms of Vaginal Atrophy
According to the Cleveland Clinic, symptoms of vaginal atrophy during menopause may include:
- Thinning of the vaginal walls
- Tightening or shortening of the vaginal canal
- Lack of vaginal moisture (dryness)
- Vaginal burning or inflammation
- Pain during intercourse
- Burning with urination
- Changes in vaginal discharge
- Paleness or thinning of the labia
- Recurring urinary tract infections
- Urinary leakage or urgency
- Peeing more often at night
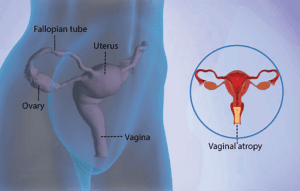
3. What Causes Vaginal Atrophy During Menopause?

Alt text: Hormonal changes impacting vaginal health during menopause
The primary cause is declining estrogen. Estrogen supports vaginal lubrication, thickness, and flexibility. Without it, the tissue becomes dry and fragile.
Additional causes:
- Surgical menopause (ovary removal)
- Breastfeeding
- Cancer treatments
- Smoking
- Lack of sexual activity (decreased blood flow)
4. 7 Empowering Ways to Treat and Manage Vaginal Atrophy
You don’t have to “just live with it.” These seven strategies can help treat and manage vaginal atrophy during menopause effectively, naturally, and confidently.
1. Use Vaginal Moisturizers
Apply non-hormonal vaginal moisturizers 2–3 times per week. These products restore hydration and help maintain pH balance.
Look for ingredients like hyaluronic acid, aloe vera, or vitamin E.
2. Stay Sexually Active
Sexual activity boosts blood circulation and keeps vaginal tissues flexible. Self-stimulation, intimacy, and vaginal dilators are all options.
🔗 Cleveland Clinic – Vaginal Dilators
3. Hydrate and Eat Hormone-Friendly Foods
Stay hydrated and eat foods that naturally support estrogen levels:
- Flaxseed, tofu, and lentils (phytoestrogens)
- Omega-3s: salmon, walnuts, chia
- Berries and leafy greens (antioxidants)
4. Practice Gentle Hygiene
Avoid scented washes, douching, and tight synthetic clothing. Choose cotton underwear and fragrance-free, pH-balanced cleansers.
5. Reduce Stress to Support Hormones
Chronic stress can worsen hormone imbalances. Gentle yoga, breathwork, and journaling can help regulate your nervous system.
6. Try Pelvic Floor Physical Therapy
A pelvic health specialist can work with you to increase blood flow and strengthen the pelvic muscles supporting vaginal wellness.
7. Avoid Smoking and Excess Alcohol
Smoking reduces estrogen and slows tissue healing. Cutting back supports better blood flow and hormonal resilience.
5. Medical Treatment Options for Vaginal Atrophy
Lifestyle changes make a big difference, but some women benefit from medical therapies.
🔹 Vaginal Estrogen Therapy
/vaginal-estrogen-rings-5113585-final-9281dcbdd27d41d3bb5f7d18b97d7103.png)

Alt text: Using vaginal estrogen ring to treat vaginal atrophy during menopause
Applied as a cream, ring, or tablet, vaginal estrogen therapy is localized and effective at restoring vaginal moisture and elasticity.
🔗 Mayo Clinic – Vaginal Estrogen
🔹 Systemic Hormone Replacement Therapy (HRT)
If you have additional menopause symptoms (e.g. hot flashes, mood changes), systemic HRT may be a helpful option. Talk to your provider to weigh the risks and benefits.
🔹 Non-hormonal prescription Medications
Ospemifene is a non-hormonal treatment that mimics estrogen’s effects in vaginal tissue without increasing systemic hormone levels.
🔹 Laser Vaginal Therapy
CO₂ or fractional lasers (like MonaLisa Touch®) help stimulate collagen and rejuvenate vaginal walls. These are especially helpful for women who cannot use hormones.
🔹 Personal Lubricants
During sex, a high-quality water- or silicone-based lubricant reduces friction and discomfort.
Avoid flavored or scented products, which can irritate sensitive tissue.
6. When to Talk to a Healthcare Provider

Alt text: Woman consulting doctor about vaginal atrophy during menopause
Reach out to a provider if you experience:
- Vaginal dryness, pain, or bleeding
- Recurring UTIs
- Discomfort with intimacy
- Urinary incontinence or urgency
You deserve answers, relief, and compassionate care.
🔗 How to Talk to Your Doctor About Menopause
7. You Deserve Comfort and Confidence
Vaginal atrophy during menopause is real, familiar, and manageable.
At MenoThrive Wellness, we empower you with culturally responsive education, tools, and support to take control of your health and feel confident in your body.
✨ You’re not alone. You’re not broken. You’re thriving.
🔗 Internal Resources:
🌐 External DoFollow Resources:
- Cleveland Clinic – Vaginal Atrophy
- NAMS – Moisturizers & Estrogen
- Mayo Clinic – Estrogen Therapy
- Drugs.com – Ospemifene